A tale of throat surgery
For the past couple of years Steve has been losing sleep.
As our previous blogs have informed and entertained you, we didn’t know what the issue was initially despite the lack of sleep, rings under his eyes, short temper and honking while sleeping.
It has been an interesting ride and process to discover what was actually going on.
A refresh
To refresh your memories and for those that don’t know, Steve suffered from severe sleep apnoea.
After numerous sleep studies, hospital stays, an extended CPAP trial, visits to specialists and much consideration the course of action decided upon was throat surgery.
For those that are interested visit;
Yes, the not-sleeping saga contines
The not-sleeping saga contines
Losing sleep over losing sleep
WARNING: the next section contains specific detailsabout Steve’s surgery which may offend or sicken.


Steve’s surgery
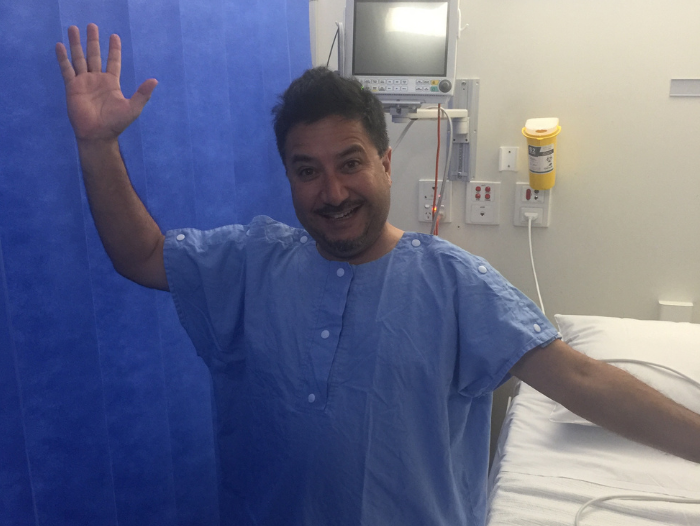
On 2 August, Steve was admitted to St John of God Hospital Subiaco and donned a smexy hospital gown for his surgery adventure.
I managed to distract myself for a couple of hours and surprisingly the miracle-worker surgeon called me to let me know the surgery went well and Steve would be coming out of the anaesthetic soon.
Post-surgery Steve was placed in ICU which looked rather serious and in actual fact it was.
The surgery involved removing a section of the back of his soft palette, his adenoids, tonsils, uvula and some of the back of his tongue.
Thus, he was in ICU to carefully monitor his airway and breathing for 12 to 24 hours.
When I first saw him he was groggy, out-of-it and had his thumb firmly pressed on the self-administering pain medication button. He was pretty out of it and couldn’t really speak.
He improved over the next 12 hours and was eventually unplugged and transferred to a general ward, although the pain medication continued of course.
“I remember eating some ice-cream and tasting charcoal,” he shared.
“Then it occurred to me that the charcoal taste was actually from my cauterised throat – ewww!”


Heading home after surgery
Hospital admissions told us he would be staying for two nights in hospital – we had expected one and so when given the choice Steve decided to come home after one night. In hindsight, he probs should have stayed because the change in temperature from a regulated hospital room to our unregulated and somewhat chilly bedroom was a shock to his throat. In other words, he didn’t sleep well.
The swelling in his throat meant he could only breath through his mouth. So, apart from having to take drugs every two hours, the air was cold to breathe and dried his mouth.
The very next day I was sent hunting and gathering, in between meetings, to find a you-beaut heater and humidifier and BINGO we were in business.
So commenced the healing process.
A note for those considering throat surgery
No matter what advice you are given or what a doctor tells you about what to expect after surgery it’s different for everyone. For Steve, he actually doesn’t remember a lot from the day of his surgery and almost two weeks afterward.
Why?
Well, the drugs he was on for that time were mega strong. He was taking a course of antibiotics, anti-inflammatories, a slow release pain killer and a mega short-term pain killer. Oh, and there were also two throat gargles, morning and night.
I’m impressed he;
- managed to swallow all of these and
- remembered to take them as and when prescribed
He actually set alarms on his phone with specific notes for what to take and do what the doctor ordered, which for someone who resists planning and structures was AMAZING!
Funny story time
Soooo…as mentioned part of the operation involved removing or cauterising the back of Steve’s tongue.
On numerous occasions during pill-swallowing-time he would swallow a pill and then become momentarily immobile before opening his mouth again, breathing out and catching the unswallowed pill in his hand. A few deep breaths and he would try again. He explained that he wasn’t sure if the pill had gone down or up. “It’s like there is a little shelf somewhere that keeps catching the pills.”
Now let me say at this point, Steve’s procedure came with a warning that food, liquid or pills could come out through the nose <insert a ‘what the?!?!? face>

Other post-surgery comments and stories include…
“Brushing my teeth is quite challenging. I’m still getting used to the feel of my tongue and how to move it. Think about what your tongue does when you brush your teeth? Well, my tongue is refusing to do that at the moment.”
“Drinking water or liquid is hard too. Not sure if it’s going to go down my throat or come out my nose!”
During the healing process Steve tried multiple pillows and sleeping positions in order to get a good night sleep but his sleep got worse before it got better.”
Eating was challenging as well. We found that a mushy baby food consistency was the best option for the first week and a bit while he relearnt how to eat, drink and swallow.
“What did you say,” Steve called out from the bedroom. ‘Nothing,’ I replied. ‘I didn’t say anything.’
“Yes, you did! I swear you were just in the room telling me something.”
YES, hallucinations were a regular occurrence during this time.
Then there’s the no.2 adventure
Can you imagine the impact taking multiple constipation-causing drugs has on the body?
Well, to put it simply, TWO WEEKS of no number 2’s is painful and blocks the toilet.
Let’s just say this was one of the things the doctor forgot to mention.
So, when all the drugs were done and dusted you would think this was the point the sleep regime would improve. No, no, no…not just yet! Believe it or not he had to struggle through 10 days’ worth of drug withdrawal involving waking every two hours ‘for a hit’ which never came, anxiety, depression, night sweats and general grumpiness.
When the annoying drug withdrawals subsided guess what happened???
A good night’s sleep!!!!

